Prostate Volume Calculator + PSA Density Calculator
References:
- Stanzione A, Ponsiglione A, Di Fiore GA, et al. Prostate Volume Estimation on MRI: Accuracy and Effects of Ellipsoid and Bullet-Shaped Measurements on PSA Density. Acad Radiol. 2021;28(8):e219-e226. doi:10.1016/j.acra.2020.05.014
- Haas M, Günzel K, Miller K, Hamm B, Cash H, Asbach P. Is the Ellipsoid Formula the New Standard for 3-Tesla MRI Prostate Volume Calculation without Endorectal Coil?. Urol Int. 2017;98(1):49-53. doi:10.1159/000448593
- Littrup PJ, Williams CR, Egglin TK, Kane RA. Determination of prostate volume with transrectal US for cancer screening. Part II. Accuracy of in vitro and in vivo techniques. Radiology. 1991;179(1):49-53. doi:10.1148/radiology.179.1.2006303
Related Calculators:
More about the Prostate Volume and PSA Density Calculator
The diagnostic approach to prostate cancer has evolved from reliance on serum prostate specific antigen (PSA) alone toward a more integrated model. This model incorporates biochemical markers, anatomical measurements, and imaging findings. While PSA remains highly sensitive, its specificity is limited by benign prostatic hyperplasia (BPH), prostatitis, and other non-malignant causes of elevation. This limitation has historically contributed to unnecessary biopsies and the detection of indolent disease with limited clinical consequence.
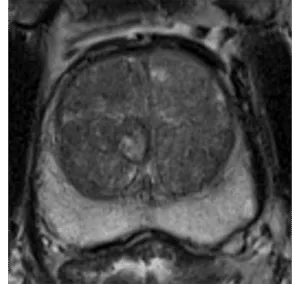
Prostate volume measurement and subsequent PSA density calculation are now central components of contemporary risk stratification. This is particularly relevant in the era of multiparametric MRI. The Prostate Volume and PSA Density Calculator offers a structured way to integrate these measurements into routine clinical workflows. By using this calculator, clinicians can better distinguish benign glandular enlargement from patterns concerning for malignancy, supporting imaging-based decision making without replacing clinical judgment.
Why is Using a Prostate Volume Calculator Important?
Prostate volume is not merely a normalization factor for PSA. It represents an independent biological variable with strong associations to cancer detection, tumor aggressiveness, and risk stratification. Numerous studies demonstrate a consistent inverse relationship between the gland size derived from a prostate volume calculator and the likelihood of clinically significant prostate cancer.
Prostate Size and Cancer Detection Rates
Small prostates, commonly defined as volumes below approximately 44 mL, are associated with substantially higher cancer detection rates. In biopsy-naive cohorts, detection rates in small glands often exceed 70%, compared with roughly one-third in larger prostates. Clinically significant cancer is more than twice as prevalent in small glands, and high-risk disease is disproportionately represented in this population.
The traditional explanation that larger glands simply dilute tumor foci has been increasingly challenged by targeted biopsy data. Even when lesions are directly targeted, detection rates remain lower in larger prostates. Within intermediate gland volumes, typically between 40 and 70 mL, each incremental 10 mL increase in prostate volume is associated with a measurable reduction in the probability of clinically significant disease.
How the PSA Density Calculator Refines Risk
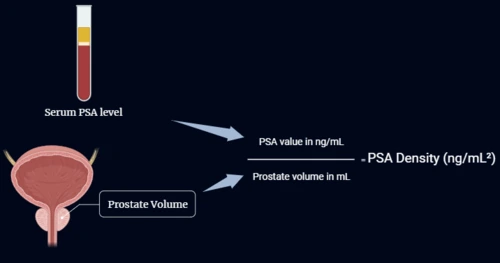
The PSA Density Calculator refines interpretation by adjusting serum PSA for gland size. It calculates this by dividing PSA by prostate volume, expressed in nanograms per milliliter per cubic centimeter (ng/mL2). This adjustment is valuable in patients with elevated PSA and equivocal imaging findings, where PSA alone may overestimate cancer risk.
PSA Density Cutoffs and Thresholds
A PSA density threshold of 0.15 ng/mL2 remains the most widely cited clinical benchmark for increased suspicion. Lower cutoffs provide strong rule-out performance. In patients with negative multiparametric MRI, a PSA density below 0.10 is associated with a very low post-test probability of clinically significant prostate cancer. Even at a cutoff of 0.15, residual risk remains limited in the absence of concerning imaging features.
PSA Density in the PI-RADS 3 "Grey Zone"
The PSA Density Calculator is especially impactful in the PI-RADS 3 assessment. In glands measuring 44 mL or larger, PI-RADS 3 lesions with low PSA density are associated with minimal risk of high-grade disease and may often be managed conservatively. In contrast, the same imaging category in a small prostate confers substantially higher risk and frequently justifies biopsy. In this context, PSA density acts as a key discriminator.
Prostate Volume Calculator Formulas: Ellipsoid vs. Bullet
Reliable measurement is the foundation of any prostate volume calculator. Most clinical workflows rely on geometric models derived from three orthogonal dimensions: length, width, and height. These measurements are typically obtained using transrectal ultrasound (TRUS) or prostate MRI.
The Ellipsoid Volume Formula (Standard)
The prolate ellipsoid formula is the most commonly implemented method in clinical software. It estimates volume as:
Volume = Length × Width × Height × 0.52
While computationally simple, this model consistently underestimates true prostate volume by approximately 17% to 18% when compared with planimetric MRI or pathological reference standards.
The Bullet Volume Formula (Alternative)
The bullet shape formula is available in this prostate volume calculator to address the geometric limitations of the ellipsoid assumption. This model represents the prostate as a composite of a cylindrical body and a hemispherical apex. The resulting constant is approximately 0.65.
Multiple studies demonstrate that the bullet formula achieves volume estimates within 10% of reference standards for most glands smaller than 55 mL. For this reason, it is often preferred when estimating prostate volume in small and moderate-sized glands, particularly when planimetric methods are impractical.
Volume Thresholds and Reference Standards
As prostate volume increases beyond approximately 55 mL, gland morphology becomes increasingly irregular due to asymmetric nodular hyperplasia. In this setting, the utility of simplified geometric formulas declines regardless of the constant used. Thin-slice MRI planimetric measurement remains the reference standard for volume estimation in large or markedly heterogeneous glands.
Integrating PSA Density With PI-RADS Assessment
The PSA density calculator complements PI-RADS assessment by adding quantitative risk stratification to qualitative imaging categories. Meta-analyses demonstrate predictable tradeoffs between sensitivity and specificity across PSA density thresholds in positive, equivocal, and negative MRI scenarios.
Lower PSA density cutoffs maximize sensitivity and negative predictive value, supporting deferral of biopsy in selected patients. Higher thresholds improve specificity at the cost of sensitivity. The optimal cutoff depends on clinical context, gland size, imaging findings, and patient-specific risk factors.
In practical application, PSA density is most valuable when MRI findings are negative or indeterminate. In clearly positive PI-RADS 4 or PI-RADS 5 lesions, biopsy is typically indicated regardless of PSA density, although the value may still provide prognostic context.
MRI vs. Ultrasound (Practical Pitfalls)
Consistent use of a prostate volume calculator requires attention to imaging technique. One common source of systematic underestimation is the "salami effect," which occurs when gland height is measured on axial images rather than in the true sagittal plane. Oblique slicing relative to the long axis leads to underestimation of height and volume. Height should always be measured orthogonal to the length measurement.
Inter-observer variability also contributes to measurement differences. Prostate MRI generally provides greater reproducibility than transrectal ultrasound, which is more susceptible to operator-dependent factors such as probe angulation and compression.
Clinical Interpretation Considerations
Impact of 5-Alpha Reductase Inhibitors: In patients receiving 5-alpha reductase inhibitors such as finasteride or dutasteride, PSA values should be adjusted (typically doubled after 6 to 12 months of therapy) to account for medication-related suppression before using the PSA density calculator.
Interpretation Context: PSA density should be interpreted alongside age-adjusted PSA reference ranges, digital rectal examination findings, MRI results, and clinical history. During active surveillance, rapid increases in PSA density or shortening PSA doubling time may warrant re-evaluation even in the absence of overt imaging progression.
Frequently Asked Questions
- How do MRI and ultrasound differ in prostate volume measurement?
Both modalities use three-dimensional measurements, but MRI provides more reliable visualization of the sagittal plane. This reduces height measurement error and improves reproducibility compared with ultrasound. - Why are 44 mL and 55 mL used as key thresholds?
A prostate volume of approximately 44 mL is associated with meaningful differences in cancer detection and aggressiveness. A threshold of 55 mL reflects a point beyond which simplified volume formulas become less reliable due to increasing gland irregularity. - When is the PSA Density Calculator more informative than PSA alone?
PSA density is particularly valuable in patients with large prostates. In these cases, PSA elevation may be driven predominantly by benign tissue rather than malignancy. - Can biopsy be deferred for PI-RADS 3 lesions?
In large glands with low PSA density, the risk of high-grade cancer is low and biopsy may often be deferred in favor of surveillance. In small glands, PI-RADS 3 lesions more commonly warrant biopsy. - Why is the bullet formula preferred for small prostates?
The ellipsoid model assumes tapering that many prostates do not exhibit. The bullet formula better reflects typical gland geometry and reduces systematic underestimation in small to mid-sized glands. - Does prostate size affect PSA levels?
Yes. Larger prostates naturally produce more PSA, which can elevate levels even in the absence of cancer. Adjusting PSA by gland volume using the PSA density calculator gives a more individualized assessment.






Thank you for this very helpful site.
Saves a lot of my reading time and improved my accuracy
please check Prostate volume calculator. The calculation tool is incorrect.
Thank you for your kind feedback Dr. Doss. The issue has been resolved.