NASCET Calculator for CTA & MRA + Report Generator
Related Calculators:
More about the NASCET Calculator
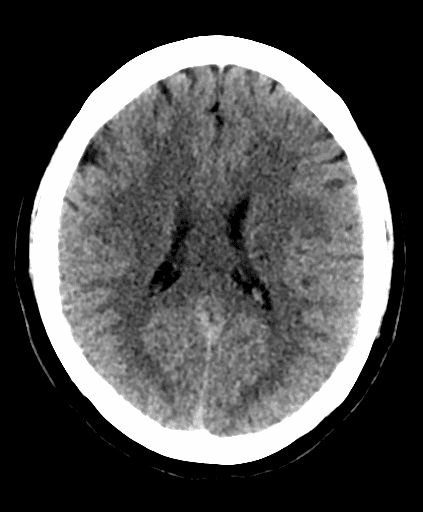
Internal carotid artery (ICA) stenosis remains a primary driver of ischemic stroke and accounts for approximately 10% of all clinical cases. Historically, the management of this disease relied on visual estimation of luminal narrowing. However, the shift toward evidence-based neurovascular practice has mandated the use of standardized quantification tools. The NASCET calculator serves as an educational resource to assist in standardizing the quantification of luminal narrowing based on the criteria established in the North American Symptomatic Carotid Endarterectomy Trial.
Precise grading of carotid stenosis is a fundamental metric used to help distinguish between patients who may benefit from aggressive medical intervention alone and those requiring surgical consideration. In modern clinical framing, physicians typically transition from the label "symptomatic carotid stenosis" to the more precise designation of a "symptomatic individual with ipsilateral carotid stenosis." This distinction underscores that the presence of a lesion does not inherently imply causality. Approximately 50% of these patients may have alternative identifiable causes for their TIA or stroke.
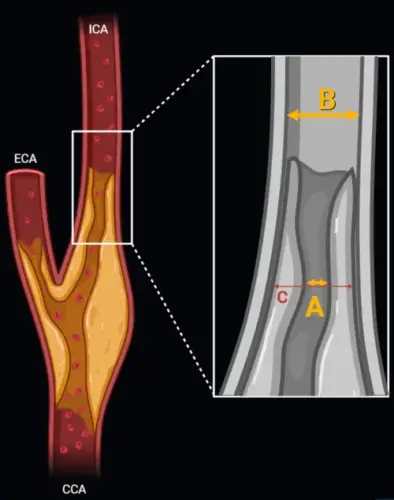
The Hemodynamic Rationale and Methodology
The carotid bulb is an anatomically complex structure characterized by a natural expansion of the arterial diameter. Simple visual estimation of this region is difficult and can lead to interobserver variability. Because the methodology used to define "normal" vessel diameter fundamentally alters the resulting percentage, a standardized approach is required to translate trial data into clinical contexts.
Over the last three decades, "Best Medical Intervention," including high-intensity statins, antiplatelet therapy, and rigorous blood pressure control, has shifted the foundations of stroke prevention. Medical intervention has reduced the annual stroke risk for asymptomatic patients with advanced stenosis to approximately 0.8%. Consequently, surgical intervention is often reserved for specific high-risk cohorts where the procedural risk is outweighed by the potential for stroke reduction.
Comparison of Angiographic Grading Methods
Accurate assessment requires a sophisticated understanding of the three primary angiographic grading systems. While each measures the residual lumen at the narrowest point, they diverge in their choice of reference points.
The NASCET Criteria (North American Standard)
The NASCET formula is defined as: (1 - [dnarrowest / ddistal]) x 100%. The reference point (ddistal) is the diameter of the post-bulbar ICA at a point where the arterial walls become parallel. Because this method uses the narrower distal ICA rather than the wider bulb, it tends to yield lower stenosis percentages compared to other systems.
The ECST Criteria (European Standard)
The ECST formula is defined as: (1 - [dnarrowest / destimated_bulb]) x 100%. This method uses the estimated diameter of the carotid bulb at the site of the lesion as the denominator. This reference point yields significantly higher percentage values than NASCET for the same lesion.
The Common Carotid (CC) Method
The CC method uses the formula: (1 - [dnarrowest / dCCA]) x 100%. The denominator is the diameter of the distal common carotid artery (CCA). Research by Staikov et al. [1] identifies this method as demonstrating high interobserver reproducibility due to the relative stability and easy visualization of the CCA reference site.
| Method | Denominator Reference Point | Clinical Reproducibility and Notes |
|---|---|---|
| NASCET | Distal post-bulbar ICA (parallel walls) | Trial standard in North America; tends to yield lower percentage values. |
| ECST | Estimated original bulb diameter | Trial standard in Europe; higher percentages; requires estimation of the bulb. |
| Common Carotid (CC) | Distal Common Carotid Artery (CCA) | High interobserver reproducibility; stable reference site; less affected by bulb morphology. |
NASCET Calculator Conversion and Inter-method Correlation
Clinicians often need to translate results between systems to apply trial data correctly. Staikov et al. [1] established mathematical relationships between these systems using linear regression:
- ECST% = (0.8 x NASCET%) + 22%
- CC% = (0.6 x NASCET%) + 39%
- ECST% = (1.2 x CC%) - 22%
For anatomical estimations where the bulb is obscured, the Carotid Stenosis Index (CSI) utilizes an anatomic constant established by Williams and Nicolaides: 1.2 x CCA diameter = proximal ICA (bulb) diameter.
Clinical Reference Correlation (70% NASCET)
A 70% NASCET stenosis corresponds to approximately 78% ECST (95% CI: 65% to 88%) and approximately 81% CC (95% CI: 73% to 92%).
Risk Stratification and Clinical Interpretation
Management paths are often defined by symptomatic status, specifically ipsilateral TIA or stroke within 6 months.
Symptomatic Benefit (CEA)
Benefit is time-dependent. In women with 70% to 99% stenosis and men with 50% to 69% stenosis, the benefit of surgery falls rapidly after 14 days and effectively disappears in women beyond this window. Men with 70% to 99% stenosis show benefit up to 3 months, though the maximum gain is within the first 2 weeks [4].
Asymptomatic Benefit (CEA)
Surgical benefit is generally established for patients with greater than 60% (ACAS) or 70% (ACST-1) stenosis who have a life expectancy of at least 5 years and are otherwise at low surgical risk [2].
| Category | Percent Stenosis (NASCET) | Management Consideration |
|---|---|---|
| Low | 0% to 29% | Aggressive medical management and risk factor modification. |
| Medium | 30% to 69% | Vigilant medical therapy. CEA benefit limited to specific symptomatic men (50% to 69%) within 14 days. |
| Severe | 70% to 99% | Surgical consideration for symptomatic patients. Medical management for most asymptomatic patients. |
| Near Occlusion | (Angiographic Collapse) | Evidence of reduced distal flow (string sign). NASCET criteria cannot be applied here as the collapsed distal ICA makes the denominator artificially small. |
Frequently Asked Questions (FAQs)
Why does the NASCET method often yield lower percentages than ECST?
NASCET uses the distal post-bulbar ICA as the denominator, whereas ECST uses the wider estimated bulb. A larger denominator in the ECST formula naturally results in a higher percentage of stenosis for the same residual lumen.
Can I use the NASCET calculator for Ultrasound-based measurements?
Yes, but you must use velocity-to-diameter correlations. A PSV of 200 cm/s or greater, or an EDV Index of 8.2 or greater, are high-yield markers for identifying stenosis that corresponds to 70% or more on the NASCET scale.
What is the clinical significance of "Near Occlusion" in NASCET grading?
In near-occlusion, the distal ICA collapses. This "collapsed denominator" prevents the accurate application of NASCET criteria, as the math will grossly underestimate the severity of the lesion. Surgical efficacy in these cases is significantly diminished.
How should I handle a discrepancy between CTA and Ultrasound results?
Discrepancies often arise because ultrasound may overestimate stenosis based on high velocities. If modalities disagree, the consultant should favor the modality most faithful to NASCET anatomy (CTA/DSA) or consider a third modality like Carotid MRA.
Is luminal narrowing the only metric for CEA eligibility?
No. Symptomatic status, the 14-day window since the last event, and the response to medical therapy are critical factors. An asymptomatic patient below the 60% threshold is generally managed with medical intervention alone.
Does the NASCET calculator account for plaque morphology?
No. The calculator is strictly a measure of luminal diameter. High-risk features like intraplaque hemorrhage must be assessed via MRI.
References
- Staikov IN, Nedeltchev K, Arnold M, et al. Comparison of the ECST, CC, and NASCET grading methods and ultrasound for assessing carotid stenosis. J Neurol. 2000;247(9):681-686. View Source
- Abbott AL. Extra-Cranial Carotid Artery Stenosis: An Objective Analysis of the Available Evidence. Front Neurol. 2022;13:738546. View Source
- Saba L, Mossa-Basha M, Abbott A, et al. Quantifying Carotid Stenosis: History and Current Applications. Life (Basel). 2024;14(2):189. View Source
- Rothwell PM, Eliasziw M, Gutnikov SA, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361(9352):107-116. View Source





this was the best nascet calculator that i saw but no longer works. not showing the % stenosis. shame
Thank you for your feedback. Over the past few days, we have encountered occasional and temporary issues due to the relocation and upgrade of our servers. I expect the website to stabilize within a day or two. Thank you for your patience.
glad to see it back up and running. the other calculators were okay but you have to click calculate instead of doing it automatically