NASCET Calculator (+ECST) for Carotid Artery Stenosis
Using measurements on CTA and MRA
References:
- North American Symptomatic Carotid Endarterectomy Trial Collaborators, Barnett, H. J. M., Taylor, D. W., Haynes, R. B., Sackett, D. L., Peerless, S. J., Ferguson, G. G., Fox, A. J., Rankin, R. N., Hachinski, V. C., Wiebers, D. O., & Eliasziw, M. (1991). Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. The New England journal of medicine, 325(7), 445–453. https://doi.org/10.1056/NEJM199108153250701
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). (1998). Lancet (London, England), 351(9113), 1379–1387.
Related Calculators:
More about the ECST & NASCET Calculator:
The North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) have served as cornerstones in the evaluation and management of internal carotid artery (ICA) stenosis. These landmark clinical trials provided robust evidence for the use of carotid endarterectomy (CEA) in symptomatic patients and fundamentally shaped modern stroke prevention strategies. Accurate quantification of ICA stenosis, as outlined by the NASCET and ECST methodologies, is now an essential part of vascular imaging and decision-making in neurovascular care.
The NASCET was a randomized, multicenter study conducted in the United States and Canada. It focused on patients with recent symptoms such as hemispheric transient ischemic attacks (TIAs), amaurosis fugax, or nondisabling ischemic strokes. The trial demonstrated that CEA dramatically reduced the risk of recurrent ipsilateral stroke in patients with high-grade ICA stenosis. In patients with 70–99% stenosis, the two-year risk of any ipsilateral stroke was 26% in those managed medically, compared to only 9% in those who underwent surgical intervention. This translated into an absolute risk reduction of 17% and a relative risk reduction of nearly 65%. Even more striking was the benefit for major or fatal strokes, with an absolute risk reduction of 10.6%. These results cemented the role of CEA as a life-saving procedure in selected patients.
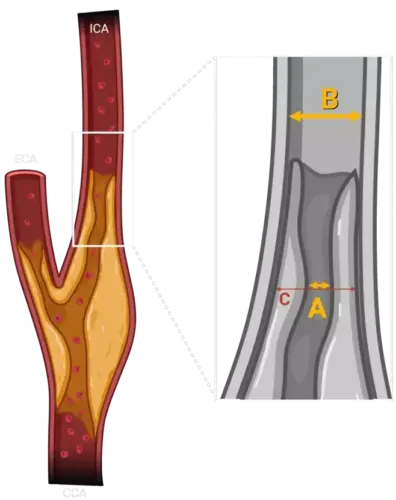
The method used in NASCET to calculate the degree of stenosis involves comparing the diameter of the most narrowed segment of the ICA with the diameter of the normal distal ICA beyond the bulb. This standardized method provided a reproducible, imaging-based formula for quantifying ICA stenosis:
Stenosis (%) = [(1 - (diameter at site of stenosis / diameter of normal distal ICA)) × 100]
The ECST, conducted in Europe, used a slightly different approach to measuring stenosis, comparing the narrowed lumen to the estimated original diameter of the artery at the site of the lesion. While this led to slightly different numerical values for the same anatomical stenosis, both trials highlighted the clinical significance of high-grade stenosis and the benefits of surgical intervention. ECST findings showed that in patients with stenosis greater than 80%, the three-year risk of major stroke or death was significantly reduced in the surgical group (14.9%) compared to the control group (26.5%), amounting to an absolute benefit of 11.6%. These outcomes reinforced the urgency of intervention in symptomatic patients and supported the global adoption of CEA in stroke prevention guidelines.
To facilitate clinical translation of these findings, we developed the NASCET calculator to automate the process of stenosis measurement and stroke risk stratification based on angiographic imaging. Whether derived from computed tomography angiography (CTA) or magnetic resonance angiography (MRA), the calculator provides a consistent method for quantifying ICA stenosis using the NASCET criteria. By generating a clear, objective percentage of stenosis, the tool supports accurate decision-making for interventions such as CEA or carotid artery stenting (CAS), ensuring that patients receive timely and evidence-based care.
In parallel, the ECST calculator was created to reflect the methodology and insights of the European trial, allowing clinicians to apply the ECST criteria where appropriate. This tool can be especially useful when comparing findings across historical datasets, when prior measurements used ECST-style calculations, or in clinical contexts where the estimated normal arterial diameter is more easily derived.
By integrating these calculators into clinical workflows, healthcare providers can:
- Standardize Assessment: Eliminate variability in stenosis calculation by using trial-validated formulas.
- Improve Workflow Efficiency: Save time by automating a crucial step in the diagnostic and treatment process.
- Facilitate Shared Decision-Making: Communicate stroke risk and treatment rationale more effectively with patients and families.
- Support Multidisciplinary Care: Provide vascular surgeons, neurologists, and radiologists with a common, evidence-based language for decision-making.
Importantly, these tools are not limited to surgical candidacy assessment. In modern practice, they are also useful in evaluating patients for carotid artery stenting (CAS), particularly in those considered high-risk for open surgery. Furthermore, they can help guide decisions in asymptomatic patients with high-grade stenosis, where management strategies remain nuanced and individualized.
While the calculators are powerful tools, it is essential to recognize their limitations. They are dependent on the accuracy of imaging measurements and are intended to complement, not replace, clinical judgment. Factors such as plaque morphology, patient comorbidities, life expectancy, and surgical risk must also be weighed carefully. Furthermore, newer imaging techniques and evolving evidence may gradually refine the thresholds for intervention over time.
Ultimately, the NASCET and ECST calculators represent a synthesis of clinical evidence, radiologic precision, and user-friendly design. By embedding them into clinical routines, we help ensure that decisions about carotid revascularization are grounded in the best available data, improving patient outcomes and advancing the standard of care in stroke prevention.




this was the best nascet calculator that i saw but no longer works. not showing the % stenosis. shame
Thank you for your feedback. Over the past few days, we have encountered occasional and temporary issues due to the relocation and upgrade of our servers. I expect the website to stabilize within a day or two. Thank you for your patience.
glad to see it back up and running. the other calculators were okay but you have to click calculate instead of doing it automatically
I do accept as true with all the ideas you’ve introduced to your post. They are very convincing and will definitely work. Still, the posts are too brief for starters. Could you please prolong them a bit from subsequent time? Thank you for the post.